Резюме
Актуальність. Хронічна хвороба нирок (ХХН) на сьогоднi є незаперечним глобальним суспільним пріоритетом. Незважаючи на те, що поширеність ХХН і її вплив на здоров’я вивчалися в основному в економічно розвинених країнах, тягар цього захворювання ще більший в країнах, що розвиваються. Мета дослідження: вивчення структури серцево-судинних патологій у пацієнтів із хронічною хворобою нирок V стадії, які отримують програмний гемодіаліз, серед міського населення Республіки Узбекистан. Матеріали та методи. Під час наукового дослідження були обстежені 104 пацієнти, які постійно проживають в м. Ташкент. Середній вік пацієнтів становив 49,7 ± 11,7 року. У дослідження були включені пацієнти з клінічно встановленим діагнозом ХХН V стадії в результаті нефропатій різного генезу. Швидкість клубочкової фільтрації розраховували, грунтуючись на концентрації креатиніну в сироватці за формулою CKD-Epi. Сеанси гемодіалізу проводили за схемою 4 години 3 рази на тиждень. Результати. За результатами дослідження 104 пацієнтів у 62 (59,6 %) обстежених була виявлена серцево-судинна патологія. Найчастіше зустрічається артеріальна гіпертензія, від неї страждали майже 53 % (n = 55) пацієнтів. Стабільна стенокардія напруження була діагностована в 38,5 % (n = 40) обстежених. Хронічна серцева недостатність виявлена в понад 19 % (n = 20) пацієнтів. Висновки. На підставі аналізу даних 104 пацієнтів із ХХН на програмному гемодіалізі можна припустити, що основними патологіями серцево-судинної системи у хворих міського населення були хронічна серцева недостатність, артеріальна гіпертензія, стенокардія напруження й різні аритмії. Можна зробити висновок, що коморбідна патологія серцево-судинної системи займає провідне місце в структурі серцево-судинних уражень у пацієнтів із хронічною хворобою нирок термінальної стадії, які отримують програмний гемодіаліз, і суттєво не відрізнялася в статевому розрізі. Також можна відзначити високу частоту цукрового діабету в обстежуваних пацієнтів із серцево-судинними захворюваннями, що відповідає літературним даним.
Актуальность. Хроническая болезнь почек (ХБП) в настоящее время является неоспоримым глобальным общественным приоритетом. Несмотря на то, что распространенность ХБП и ее влияние на здоровье изучались в основном в экономически развитых странах, бремя этого заболевания еще больше в развивающихся странах. Цель исследования: изучение структуры сердечно-сосудистых патологий у пациентов с хронической болезнью почек V стадии, получающих программный гемодиализ, среди городского населения Республики Узбекистан. Материалы и методы. В ходе научного исследования были обследованы 104 пациента, постоянно проживающих в г. Ташкенте. Средний возраст пациентов составил 49,7 ± 11,7 года. В исследование были включены пациенты с клинически установленным диагнозом ХБП V стадии в результате нефропатий различного генеза. Скорость клубочковой фильтрации рассчитывали, основываясь на концентрации креатинина сыворотки по формуле CKD-Epi. Сеансы гемодиализа проводили по схеме 4 часа 3 раза в неделю. Результаты. По результатам исследования 104 пациентов у 62 (59,6 %) обследованных была обнаружена сердечно-сосудистая патология. Самой частой оказалась артериальная гипертензия, ею страдали почти 53 % (n = 55) пациентов. Стабильная стенокардия напряжения была диагностирована у 38,5 % (n = 40) обследованных. Хроническая сердечная недостаточность была выявлена у более чем 19 % (n = 20) пациентов. Выводы. На основании анализа данных 104 пациентов с ХБП на программном гемодиализе можно предположить, что основными патологиями сердечно-сосудистой системы у больных городского населения являлись хроническая сердечная недостаточность, артериальная гипертензия, стенокардия напряжения и различные аритмии. Можно сделать вывод, что коморбидная патология сердечно-сосудистой системы занимает ведущее место в структуре сердечно-сосудистых заболеваний у пациентов с хронической болезнью почек терминальной стадии, получающих программный гемодиализ, и существенно не отличается в половом разрезе. Также можно отметить высокую частоту сахарного диабета у обследуемых пациентов с сердечно-сосудистыми заболеваниями, что соответствует литературным данным.
Background. Chronic kidney disease (CKD) is now an undeniable global public priority. Although the prevalence and health effects of CKD have been studied primarily in economically developed countries, the burden of the disease is even greater in developing countries. For this purpose, we decided to study the structure of cardiovascular pathologies in patients with stage 5 chronic kidney disease receiving programmed hemodialysis of the urban population. Materials and methods. In the course of the scientific study, 104 patients permanently residing in the city of Tashkent were examined. The average age of the patients was 49.7 ± 11.7 years. The study included patients with a clinically established diagnosis of stage 5 CKD due to nephropathies of various origins. Glomerular filtration rate was calculated based on serum creatinine concentration using the CKD-Epi formula. Hemodialysis sessions were carried out according to the scheme 4 hours 3 times a week. Results. According to the results of a study of 104 patients, 62 (59.6 %) of the examined had cardiovascular pathology. The most frequent occurrence was arterial hypertension, almost 53 % (n = 55) of patients suffered from it. Stable angina was detected in 38.5 % patients (n = 40). Chronic heart failure was found in more than 19 % (n = 20) of patients. Conclusions. The results of the analysis of 104 CKD patients on hemodialysis demonstrated that the main pathologies of the cardiovascular system in urban patients were chronic heart failure, arterial hypertension, angina, and various arrhythmias. It can be assumed that the comorbid pathology of the cardiovascular system dominates in the structure of cardiovascular lesions in patients with end-stage chronic kidney disease receiving programmed hemodialysis and is not sex-related. It also may be noted the high incidence of diabetes mellitus in the examined patients with cardiovascular disease, which corresponds to the literature data.
Introduction
In a recently published joint report by the European Renal Association-European Dialysis and Transplant Association, American Society of Nephrology, and International Society of Nephrology, kidney diseases were recognized as one of the most common diseases in the world [1]. According to this report, globally, the total number of people with chronic kidney disease (CKD), acute kidney injury and people receiving renal replacement therapy exceeds 850 million, which is actually twice the estimated number of patients with diabetes mellitus around the world and 20 times higher than the number of people suffering from acquired immunodeficiency syndrome/human immunodeficiency virus worldwide. CKD is currently an undeniable global public priority [2, 3].
Despite the fact that the prevalence of CKD and its effects on health have been studied mainly in economically developed countries, the burden of this disease is even greater in developing countries [4, 5].
The risk of cardiovascular complications increases inversely with the level of glomerular filtration rate (GFR), and with GFR < 30 ml/min exceeds that with preserved renal function 5.5 times. A significant number of patients with CKD die due to cardiovascular complications even before the end-stage renal disease [6].
In patients with essential arterial hypertension (AH) without any cardiovascular complications, a moderate decrease in GFR is accompanied by a doubling of the risk of cardiac death. International recommendations on hypertension unconditionally recognize microalbuminuria (MAU) and a decrease in GFR as some of the main risk factors for the progression of cardiovascular disease [7, 8].
Besides, it turned out that in the general population aged 45–74 years, a decrease in GFR below 60 ml/min acts as an independent risk factor for acute myocardial infarction, general and cardiovascular mortality [9].
Also, to date, a lot of literature has been accumulated on the role of proteinuria, MAU in the progression of renal pathology and cardiovascular disease (CVD) [10, 11]. In fact, the prevalence of albuminuria, both micro- and macro-, increases with a drop in GFR < 60 ml/min/1.73 m2 [12]. MAU is believed to reflect the presence of generalized endothelial dysfunction in the body, which, in turn, is the cause of accelerated atherogenesis and progression of renal fibrosis [13].
Scientific research is widely conducted to study the place of ischemic heart disease (IHD) in the structure of CVD and its course in patients with CKD [14, 15]. So, in a prospective study of V.A. Dobronravov et al. (2002–2009), a detailed long-term clinical analysis of the course of myocardial ischemia (MI) was performed in 119 patients on hemodialysis. At the time of inclusion in the study, clinical signs of MI were detected in 60 (50.4 %) patients, of which typical angina pectoris in 52 %, painless MI in 23 % (the prevalence of painless MI was even greater than in patients with diabetes mellitus and was likely to be due to the presence of neuropathy against the background of persistence of uremia, as well as damage to the intramyocardial arteries), a mixed form in 25 %. Among 66 out of 119 patients who had cardiovascular events, mortality was 59 %, the total proportion of patients with some form of MI was 86 %, and MI progression was observed in 82 %. In 35 % of the latter, clinical signs of coronary insufficiency first appeared during the observation period. An unexpected result of the work was also the discovery of the association of higher values of troponin T (TnT) with the presence of MI signs at the time of inclusion of patients in the study. Since cases of acute coronary syndrome in patients were completely excluded at the beginning of a prospective observation, the authors suggested that this marker reflects the development of deeper chronic damage to myocardiocytes caused by MI in dialysis patients. This indicator was also an independent predictor of death from CVD: at TnT > 0.05 ng/ml, the relative risk of cardiac death increased 5 times. Also, the relationship between a decrease in diastolic blood pressure on the first post-dialysis day, a higher level of plasma homocysteine and the progression of MI was shown. Considering the data obtained, the authors indicate the need for a thorough examination of patients for the presence of MI at the beginning of renal replacement therapy or when planning it. Moreover, the onset or progression of coronary heart disease is characteristic of the early period after the onset of hemodialysis [15].
A number of studies have investigated the frequency of valve calcification in patients with CKD: calcification of heart valves among dialysis patients occurs in 20–78 % cases and calcification of the mitral valve fibrous ring in 31–46 %. According to M.M. Volkov et al., at the pre-dialysis stage of CKD, valve calcification was detected in 22.1 % of patients. Thus, the frequency of valve calcification increases with the CKD progression, reaching a maximum in the dialysis population [16].
The studies have also investigated the problems of cardiovascular lesions in patients with CKD on hemodialysis in different populations. In particular, the urban and rural population was studied and distinctive data have been obtained that show the relevance of studying this problem [17].
The purpose of the study was to investigate the structure of cardiovascular pathologies in patients with stage 5 chronic kidney disease receiving programmed hemodialysis of the urban population of the Republic of Uzbekistan.
Materials and methods
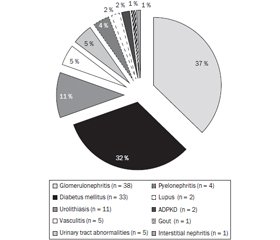
During the scientific study, there were examined 104 patients permanently residing in the city of Tashkent. The study was conducted in hemodialysis departments of the Republican Specialized Scientific and Practical Medical Center of Nephrology and Kidney Transplantation and the Republican Specialized Scientific and Practical Medical Center of Urology during 2018. Forty-nine per cent (n = 51) of the examined patients were men and 51 % (n = 53) were women. The average age of the patients was 49.7 ± 11.7 years. The study included patients with a clinically established diagnosis of CKD stage 5 (according to NKF KDOQI 2002) in the outcome of nephropathies of various origins. Glomerular filtration rate was calculated based on the serum creatinine concentration according to the formula CKD-Epi. The classification of blood pressure levels and the definition of hypertension were determined according to the Recommendations for the management of arterial hypertension of the European Society of Cardiology and the European Society of Arterial Hypertension of 2018 [18]. The main underlying diseases were chronic glomerulonephritis (n = 38), diabetes mellitus (n = 33), urolithiasis (n = 11), systemic vasculitis (n = 5), developmental abnormalities and pathology of the urinary tract (n = 5), chronic pyelonephritis (n = 4), systemic lupus erythematosus (n = 2), polycystic kidney disease (n = 2), interstitial nephritis (n = 1), and gout (n = 1) (Fig. 1). The duration of hypertensive disease was 37 (6–89) months. The length of stay in the hospital was at least 10 days. Programmed hemodialysis was performed with Fresenius Medical Care 4008S, WEGO F15 LW, and Diacap Polysulfone LOPS18 LW dialyzers. Hemodialysis sessions were performed according to the scheme 4 hours 3 times a week. For hemodialysis, a bicarbonate solution was used as a dialysate. Kt/V indicators corresponded to a minimum target level of 1.4. Criteria for exclusion from the study were under 18 years of age, rural residents, patients who underwent kidney transplantation, patients receiving HD in acute renal failure. The examination program included general clinical laboratory research. Biochemical analysis indices were determined using a Mindray RS-200 automatic biochemical analyzer; HumaClot Junior analyzer was used to determine coagulation indices. To study the state of the cardiovascular system, all patients underwent blood pressure monitoring, electrocardiography, and echocardiography. Electrocardiography was performed on an apparatus MIDID-EK1T. Echocardiography was performed at the Republican Specialized Scientific and Practical Medical Center for Therapy and Medical Rehabilitation on ultrasonic devices Samsung Medison Accuvix V20.
Statistical data processing was carried out using the standard Statistica for Windows package, version 6.0. The Mann — Whitney test was used to compare two independent groups, the Kruskal — Wallis test was used to compare more than two independent groups, the Spearman’s correlation coefficient was used for correlation analysis, and multiple linear regression analysis was also performed. Differences were considered significant at p < 0.05.
Results and discussion
According to the results of a study of 104 patients, cardiovascular pathology was detected in 62 (59.6 %) examined. Arterial hypertension turned out to be the most frequent cardiovascular pathology, almost 53 % (n = 55) of patients suffered from it (Table 1). The number of patients with IHD (stable angina pectoris) turned out to be slightly less — 38.5 % (n = 40) of the examined. Heart failure (HF) was detected in more than 19 % (n = 20) of patients. Rhythm and conduction disorders were also observed: atrial fibrillation was detected in 3 (2.9 %) examined patients, ventricular extrasystoles were diagnosed in 2 (1.9 %) patients, and 2 (1.9 %) patients were diagnosed with the complete blockade of the His left bundle. During the examinations, one (1 %) patient was diagnosed with focal myocarditis. Also, one patient had acquired heart disease; according to echocardiography, he was diagnosed with mitral heart disease, with a predominance of stenosis. Diabetes mellitus occurred in 32 % (n = 33) of the examined patients. Left ventricular hypertrophy on echocardiography was observed in 79 patients. It should be noted that blood pressure parameters reliably correlate with left ventricular hypertrophy. The data obtained found that almost 77 % of patients (n = 80) were diagnosed with renal anemia.
/14.jpg)
The results of the analysis demonstrated the following distribution of the main cardiovascular pathologies related to severity and gender. Arterial hypertension was observed in 55 (57 %) patients (27 men and 28 women). Besides, more than half of them (32 (58.2 %)) had grade 2 arterial hypertension; 5 (9.1 %) patients had grade 1 hypertension, grade 3 hypertension was observed in 18 (32.7 %) patients (Fig. 1). It should be noted that all 5 patients with grade 1 AH were women. Grade 2 AH was more common in men (n = 17) than in women (n = 15), grade 3 AH was more often observed in men — 55.5 % (Fig. 2). The average systolic blood pressure was 151 ± 18 mm Hg, the average diastolic blood pressure was 86 ± 13 mm Hg.
Angina pectoris was diagnosed in 40 (38.5 %) examined patients who noted complaints characteristic for stable angina pectoris. When distributing patients according to functional classes (FC), according to the classification of the Canadian Cardiovascular Society (L. Campeau, 1976), there was a lack of FCI angina in the examined patients (Fig. 3), as well as FCIV angina in women. 52.5 % (n = 21) patients with angina pectoris were diagnosed with FCII (12 men and 9 women). Angina of functional class III (n = 17) was more often diagnosed in women (64.7 %) than in men (35.3 %). FCIV was determined only in 2 men (Fig. 3).
Chronic heart failure was diagnosed in 20 (19.2 %) examined patients (Fig. 4). Patients were divided according to the functional classes (by NYHA, 1964). Not a single patient was diagnosed with chronic heart failure (CHF) FCI. Only one (1.4 %) patient (male) was diagnosed with CHF FCIV. Eleven (10.6 %) of the examined patients, of which 7 men, 4 women, described complaints typical for CHF FCII (Fig. 4). Eight (11.1 %) of the examined patients were diagnosed with CHF FCIII (4 men and 4 women).
It should be noted that most of the examined patients showed comorbidity of cardiovascular diseases. The most frequent comorbid state was found in angina, hypertension and heart failure in various combinations.
It was found that all patients (n = 40) who were diagnosed with stable angina pectoris also had chronic heart failure and/or arterial hypertension. Thirteen (12.5 %) of the examined patients had a combination of angina + AH + HF. The combination of angina + AH was observed in 26 (25 %) patients. Fourteen patients had isolated arterial hypertension, only 2 patients had a combination in the form of AH + HF.
According to the above data, chronic heart failure turns out to be also more common in a comorbid state. For example, if angina + AH + HF is almost 70 % (n = 14) of the number of cases with HF, then AH + HF occurs in 5 % (n = 1) of patients with HF. And only 20 % (n = 4) of patients with heart failure did not have other cardiovascular pathologies. In terms of sex, the comorbidity of cardiovascular pathology did not significantly differ between both sexes. For example, the combination of angina + AH + HF and angina + AH was almost identical, 6 men and 6 women, 13 men and 13 women, respectively. If isolated cases of AH were found only in women (n = 2), then isolated CHF was more common in men (n = 3) than in women (n = 1).
A combination of several types of different arrhythmias was also observed, which is typical for this population according to published data [19]. For example, of three patients who were diagnosed with atrial fibrillation, two had also ventricular extrasystoles. Given that the number of cases with ventricular extrasystoles was only 2, it is not difficult to notice that all patients with ventricular extrasystoles had also atrial fibrillation.
Since today diabetes mellitus is considered as the equivalent of the presence of a clinically expressed cardiovascular disease in the patient and an independent CVD risk factor [20], it was also interesting to study the presence of diabetes mellitus in the examined patients with cardiovascular pathology. As a result of the study, it was revealed that out of 62 patients with cardiovascular pathology, diabetes mellitus was diagnosed in 26 (42 %) patients.
As known [21], long-term anemia may be accompanied by an enlargement of the left heart and the development of CVD. Based on this, it should be noted that 77 % of the patients with cardiovascular pathology examined by us experienced anemia. In our group of patients, it was presented with renal anemia, which is typical for patients with CKD stage 5 [22].
Conclusions
Cardiovascular complications dominate among pathologies in patients with CKD on programmed dialysis [23]. Based on the analysis of 72 CKD patients on programmed HD, it can be assumed that the main pathologies of the cardiovascular system in patients were chronic heart failure, hypertension, angina pectoris and various arrhythmias. A particularly high frequency of occurrence was observed in pathologies such as angina and AH, which roughly corresponds to international studies [24].
According to the above results of our study, it can be assumed that the comorbid pathology of the cardiovascular system dominates in the structure of cardiovascular lesions in patients with end-stage chronic kidney disease receiving programmed hemodialysis and did not significantly differ by sex. Also, a high incidence of diabetes mellitus in the examined patients with CVD can be noted, which is consistent with published data [23].
Conflicts of interests. Authors declare the absence of any conflicts of interests and their own financial interest that might be construed to influence the results or interpretation of their manuscript.
Information about the contribution of each author: Daminov B.T. — study concept and design; Yarygina S.V. — collection and processing of materials; Sharapov O.N. — collection and processing of materials. Analysis of the received data, writing text.
Список литературы
1. Jager K.J. et al. A single number for advocacy and communication — worldwide more than 850 million individuals have kidney diseases. Nephrology Dialysis Transplantation. 2019. Vol. 34. No 11. P. 1803-1805. doi: 10.1093/ndt/gfz174.
2. Levin A., Tonelli M., Bonventre J. et al. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet. 2017. 390. P. 1888-1917. doi: 10.1016/S0140-6736(17)30788-2.
3. Crews D.C., Bello A.K., Saadi G. et al. Burden, access, and disparities in kidney disease. Kidney International. 2019. 95. P. 242-248. doi: 10.1016/j.kint.2018.11.007.
4. Hill N.R., Fatoba S.T., Oke J.L. et al. Global prevalence of chronic kidney disease — a systematic review and meta-analysis. PLoS One. 2016. 11. doi: 10.1371/journal.pone.0158765.
5. Xie Y., Bowe B., Mokdad A.H. et al. Analysis of the global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney International. 2018. 94. P. 567-581. doi: 10.1016/j.kint.2018.04.011.
6. Gruberg L. et al. Comparison of outcomes after percutaneous coronary revascularization with stents in patients with and without mild chronic renal insufficiency. American Journal of Cardiology. 2002. Vol. 89. P. 54-57. doi: 10.1016/s0002-9149(01)02163-4.
7. Mancia G. Guidelines for the Management of Arterial Hypertension. Journal of Hypertension. 2007. Vol. 25. P. 1105-1187. doi: 10.1097/HJH.0000000000000466.
8. Tonelli M. et al. Chronic kidney disease and mortality risk: a systematic review. Journal of American Society of Nephrology. 2006. Vol. 17. P. 2034-2047. doi: 10.1681/ASN.2005101085.
9. Meisinger C. et al. Сhronic kidney disease and risk of incident myocardial infarction. European Heart Journal. 2006. Vol. 27. P. 1245-1250. doi: 10.1093/eurheartj/ehi880.
10. Forman J.P., Brenner B.M. ‘Hypertension’ and ‘microalbuminuria’: the bell tolls for thee. Kidney Int. 2006. 69 (1). 22-28. doi: 10.1038/sj.ki.5000056.
11. Redon J., Williams B. Microalbuminuria in essential hypertension: redefining the threshold. J. Hypertens. 2002. 20 (3). 353-355. doi: 10.1097/00004872-200203000-00002.
12. Sarafidis P.A., Bakris G.L. Microalbuminuria and chronic kidney disease as risk factors for cardiovascular disease. Nephrol. Dial. Transplant. 2006. 21 (9). 2366-2374. doi: 10.1093/ndt/gfl309.
13. Smirnov A.V., Dobronravov V.A., Kayukov I.G. Cardiorenal continuum, pathogenetical grounds of preventive nephrology. Nephrology (Saint-Petersburg). 2005. 9 (3). P. 7-15. (In Russian).
14. Sánchez-Perales C., Vázquez-Ruiz de Castroviejo E., Segura-Torres P. et al. Incidence of acute myocardial infarction in the evolution of dialysis patients. Nefrologia. 2012. 32 (5). P. 597-604. doi: 10.3265/Nefrologia.pre2012.Jun.11464.
15. Dobronravov V.A. et al. Myocardial ischemia in patients on maintenance haemodialysis: results of 7-year prospective observational study. Nephrology (Saint-Petersburg). 2013. 17 (1). P. 45-49. (In Russian).
16. Volkov M.M. et al. Atherosclerosis as the main factor of calcinosis of the heart valve apparatus in the predialysis period of chronic kidney disease. Nephrology (Saint-Petersburg). 2007. 11 (4). P. 47-54. (In Russian).
17. George J.A., Brandenburg J.T., Fabian J. et al. Kidney damage and associated risk factors in rural and urban sub-Saharan Africa (AWI-Gen): a cross-sectional population study. Lancet Glob. Health. 2019. 7 (12). e1632-e1643. doi: 10.1016/S2214-109X(19)30443-7.
18. Williams B., Mancia G., Spiering W. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension [published correction appears in Eur. Heart J. 2019 Feb 1. 40 (5). 475]. Eur. Heart J. 2018. 39 (33). P. 3021-3104. doi: 10.1093/eurheartj/ehy339.
19. Pun P.H. et al. Characteristics of cardiac arrest and bystander resuscitation within outpatient dialysis clinics in North Carolina. Journal of the American College of Cardiology. 2018. Vol. 71. No 11. P. 303. doi: 10.1016/S0735-1097(18)30844-1.
20. Ametov A.S., Kurochkin I.O., Zubkov A.A. Saharnyj diabet i serdechno-sosudistye zabolevanija. Rossijskij medicinskij zhurnal. 2014. No 13. P. 954-963. (In Russian).
21. Budnevsky A.V., Ovsyannikov E.S., Redka A.V. The influence of anemia on cardiovascular disease course. Cardiovascular Therapy and Prevention. 2016. 15 (1). P. 64-68. (In Russian). doi: 10.15829/1728-8800-2016-1-64-68.
22. Fouad S. Cost effectiveness of darbepoetin alfa versus epoetin alfa in the management of anemic patients with chronic kidney disease: health insurance perspective. Value in Health. 2016. Vol. 19. P. A589. doi: 10.1016/j.jval.2016.09.1394.
23. Sharapov O.N. Serdechno-sosudistye oslozhnenija u bol'nyh, s hronicheskoj bolezn'ju pochek, poluchajushhih programmnyj gemodializ. Nauka i zdravoohranenija. 2019. Vol. II, No 4. P. 8. (In Russian).
24. Makarov E.V., Maksudova A.N., Shakirov I.D. Status of the cardiovascular system in patients on hemodialysis. Practical medicine. 2015. Vol. 7. No 7. P. 124-129.

/14.jpg)
/15.jpg)