Журнал «Медицина неотложных состояний» 1 (64) 2015
Вернуться к номеру
Pseudomonas aeruginosa: the modern reality of antibiotic therapy
Авторы: L.A.Harchenko - Ukrainian Medical Center intensive therapy for sepsis; Department of Anesthesiology and Intensive Care Knape them. P.L.Shupyk
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
Antibiotics in medical practice today is extremely important drugs to fight bacterial infections. Introduction to the medical practice of the word "antibiotic" coincided with the opening of the first aminoglycoside streptomycin in 1944 and is owned by Nobel Prize winner Professor Waxman SD After the introduction of antibacterial perparatov into practice, they came to be regarded as medicines can cure all problems infectious diseases.
To date, the treatment of community-acquired bacterial infections most still have highly active antibiotics, but the fight against nosocomial multidrug-resistant microbes garazdo pitiable situation.
The world community has assumed widespread gram-positive microbial flora, especially methicillin-resistant. Were introduced to the pharmaceutical market: vancomycin and teicoplanin, daptomycin, linezolid, tigecycline and cephalosporin V generation (zinforo).
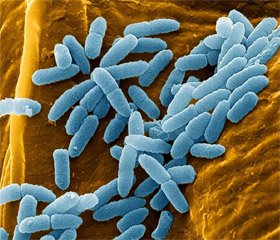
Against infections caused by gram-negative microbial flora, the range of products is significantly limited. The leader among invincibility is Pseudomonas aeruginosa.
Pseudomonas aeruginosa isolates were multiresistant when they show resistance to at least one of antibacterial drugs in three or more categories of antibiotics, resistant too, if there is resistance to at least one drug in all categories, except for one or two, and panrezistentnymi if isolate exhibits resistance to all antibiotics in all categories of antimicrobial agents. In this paper, we consider the possibility of antibiotic therapy and multi-drug-resistant over-infections caused by Pseudomonas aeruginosa.
As a rule, the initiation of antibiotic therapy is conducted empirically. The choice of antibiotic therapy for nosocomial Pseudomonas infection should be based on microbiological data of the passport, as well as the patient has risk factors for infection multiresistant pathogens.
In the Ukrainian Center for intensive therapy for sepsis (UMTSITS) for over 20 years conducted microbiological monitoring isolates isolated in the center of the various media: blood, urine, wounds et al., That provides important information for the purpose of rational antibiotic therapy, both empirically and taking into account inoculated mikrobnologicheskoy flora.
On the basis of microbiological and clinical data to be regularly updated list of antibiotics, sensitivity to which priority is determined.
Microbiological sensitivity in the heart occurs mainly disc diffusion method that allows you to change the priorities of determining the microbiological sensitivity of topical antibiotics.
Antibiotic sensitivity Ps. aur. UMСITS in 2013. n-127
It should be noted that the isolates, which determines the sensitivity to the so-called "problematic" patients, i.e. which has long been in various hospitals and received no clinical effect of antibiotic therapy.
After receiving the answer bacteriological laboratory of microbiological sensitivity of isolates must be concluded alone or in combination antibiotic therapy, but only anti-inflammatory drug is a priority kolomitsin.