Журнал «Здоровье ребенка» 2 (61) 2015
Вернуться к номеру
Annular pancreas associated with torch-infection.
Авторы: Veseliy S.V., Klimanskiy R.P., Latyshov K.V.
Donetsk National Medical University named after M.Gorky, Krasnyi Lyman, Ukraine
Разделы: Клинические исследования
Версия для печати
A group of viral, bacterial and other infections has been allocated among the most of infectious disease in 1971. These pathogens, possessing a considerable variety of structural and biological properties, cause similar clinical manifestationswhen intrauterine infection at children, and subsequently - resistant structural defects of various organs and systems. Abbreviation TORCH-complex was offered in order to indicate infections in this group [1].
The most important representatives of TORCH-complex are cytomegalovirus infection. Clinically significant forms of CMV infection can cause severe pathology, even the death of the child. [2] Even when asymptomatic forms 5-15% of children in the next 1-2 years and in later periods of life are recorded such as hearing impairment, visual, cerebral palsy, mental retardation [3]. The probability of infection of the fetus with a latent course of the process is virtually absent, with reactivation and persistence of 0.5-7.0%, while primary infection - up to 40.0% [4].
The causative agent of toxoplasmosis (Toxoplasma gondii) is a type of simple, is an intracellular parasite and has a complicated developmental cycle. Transplacental transmission of infection to the fetus is possiblefrom an infected mother during pregnancy. The number of cases of congenital toxoplasmosis fluctuates from 1 in 1,000 to 1 in 10,000 live births. At the same time, toxoplasmosis can be transmitted through blood [5].
The risk of infection and its outcome depends on the gestational age at the time of infection. The probability of transplacental transmission of Toxoplasma infection of the fetus at 8 weeks of pregnancy is 17%. The defeat of the fetus in early gestation often ends by his intrauterine death or causing serious malformations. This is due to the fact that the fetal immune system is not developed yet and is not capable toproducean immune response. The probability of infection of the fetus during infection in pregnant 8-18 weeks gestation is 25% and causes pathology of the internal organs and the brain. When the infection happens at later date the likelihood of transplacental transmission of Toxoplasma increases to 65% when the infection in 18-24 weeks gestation and up to 80% when the infection happens after 24 weeks of pregnancy. Such a high risk of fetal infection is connected with a higher permeability of the placenta in the later stages of gestation. Infection in during the later stages of intrauterine period causes the development of pathologies less pronounced the fetus and newborn, that is connected with the development of the fetus's immune system and the formation of their own immune response [6].
Congenital malformations of the digestive system occur with a frequency of 3.4 cases per 100 perinatal autopsies, and make up 21.7% of all congenital malformations in this period [7, 8]. In some defects, which are formed very early in the period of organogenesis, obstruction is developed even in utero, and the child is born with symptoms of intestinal obstruction. Some authors associate organogenesis intestinal tube with TORCH-infection [9, 10, 11].
Here is a clinical observation.
Patient S., born 01.10.2014, the 4 th of pregnancy, occurring against the backdrop toxemia of pregnancy, the threat of termination at 16 weeks. The second half of pregnancy proceeded with threatened preterm labor in 29-30 weeks. Diagnosed with uterine fibroids, polyps of the cervical canal. Childbirth II, breech presentation, Apgar score 5-6 balls. Birth weight 1350 g, height - 42 cm. At heavy birth. On the 1st day in the hospital were anxiety, vomiting, congestive contents of stomach and duodenum. Child was consulted by pediatric surgeon, anomaly of the gastrointestinal tract with symptoms of high intestinal obstructionwas suspected. Through sanaviatsii the child was brought to the intensive care unit infants Regional Children's Hospital in Donetsk.
It was severe condition of the child at the reception. Neonatal reflexes were depressed. Skin and visible mucous were net, pallor and dryness of the skinwere expressed. Elasticity of the tissues were reduced. Subcutaneous tissue was moderately developed. Peripheral lymph nodes were not enlarged. Nasal breathing was freely. Auscultation breathing in lung was weakened. Cardiac sounds were rhythmical, deaf. The boundaries of the heart were within the normal range. Belly was of acicular shape, asymmetrical due konturatsii stomach on the anterior abdominal wall, did not participate at the act of breathing. On palpation of the abdomen is soft, the act of palpation disturbed the child. Liver+3.5 cm, spleen and kidneys were not enlarged. Peristalsis was not heard. Pathological formations were not palpable. Scanty stool, urine was not broken.
In the analysis of blood - mild anemia. There were ultrasonographic signs of a moderate increase in liver. Echocardiography: congenital heart disease (atrial septal defect, patent ductus arteriosus). Consultation of the neurologist: perinatal hypoxic-ischemic brain injury, cerebral syndrome oppression.
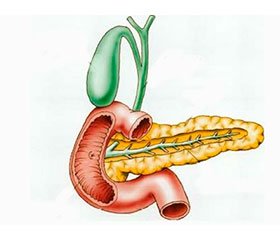
On the basis of clinical and radiological data, partial congenital high intestinal obstruction was diagnosed. After the preoperative preparation 11.01.2014 operative treatment was made. Laparotomy. The audit of the duodenum revealed that last was annularly encircled and distorted by the pancreas. Attempt to intubate the duodenum by orogastric tube was unsuccessful. Cojnsidering the compression of the duodenum annular pancreas and its deformation, it was produced imposition bypass duodenoeyunoanastomosis.
During the surgery in order to determine the DNA viruses TORCH-infections, biomaterial - the contents of the lumen of the duodenum wastaken.
Diagnosis after surgery. Multiple congenital malformations. Partial congenital high intestinal obstruction on the basis of annular pancreas. Atrial septal defect, patent ductus arteriosus. Intrauterine infection.
The result of the study of biological material, removed during surgery: DNA cytomegalovirus and toxoplasma were revealed. Thus, TORCH-infection diagnosis was confirmed.
The postoperative course was hard. Patients received an infusion, antiplatelet, nootropic, antibacterial, antiviral and symptomatic therapy. The wound healed by primary intention. After gaining weight 2500 g was discharged in satisfactory condition tothe outpatient treatment. Recommended – monitoring by immunologist, pediatric surgereon, cardiac surgereon, carrying antiviral therapy for 1 month. Assessed 2 months after surgery. Grows and develops without peculiar properties. Physical and psychomotor development is satisfactory.
This clinical observation is indicative of the associative links of TORCH-infections and congenital malformations of the gastrointestinal tract.