Журнал «Медицина неотложных состояний» Том 16, №8, 2020
Вернуться к номеру
Синдром стійкого запалення, імуносупресії та катаболізму: механізми саркопенії і шляхи корекції
Авторы: Чуклін С.М., Чуклін С.С., Шершень Г.В.
Львівська обласна клінічна лікарня, м. Львів, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
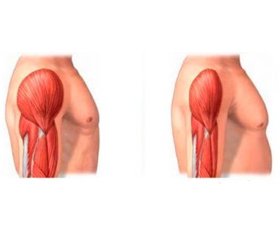
Завдяки прогресу в галузі інтенсивної терапії багато пацієнтів із тяжкою патологією виписуються з відділень інтенсивної терапії. Проте у частини хворих зберігається тривале, слабкого ступеня запалення, відновлення є затяжним, розвивається хронічний критичний стан. Крім того, у деяких пацієнтів поряд зі стійким запаленням виникають імуносупресія та катаболізм. У 2012 році цей стан був виділений в окремий синдром, який може спостерігатися після тяжкої травми й опіків, сепсису, некротичного панкреатиту. Одним із провідних клінічних проявів при цьому є значна втрата м’язової маси тіла, що погано піддається корекції. При використанні літератури з бази MedLine описано сучасні уявлення про механізми саркопенії при синдромі стійкого запалення, імуносупресії та катаболізму і можливі шляхи оптимальної анаболічної підтримки.
Благодаря прогрессу в области интенсивной терапии многие пациенты с тяжелой патологией выписываются из отделений интенсивной терапии. Однако у части больных сохраняется длительное слабой степени воспаление, восстановление является затяжным, и у них развивается хроническое критическое состояние. Кроме того, у некоторых пациентов наряду с устойчивым воспалением возникают иммуносупрессия и катаболизм. В 2012 году это состояние было выделено в отдельный синдром, который может наблюдаться после тяжелой травмы и ожогов, сепсиса, некротического панкреатита. Один из ведущих клинических проявлений при этом — значительная потеря мышечной массы тела, плохо поддающаяся коррекции. При использовании литературы из базы MedLine описываются современные представления о механизмах саркопении при синдроме устойчивого воспаления, иммуносупрессии и катаболизма и возможные пути оптимальной анаболической поддержки.
Due to advances in intensive care, many patients with severe pathology are discharged from intensive care units. However, prolonged mild degree inflammation persists in some patients, recovery is protracted, and chronic critical illness develops in them. In addition, persistent inflammation, immunosuppression and catabolism arise. In 2012, this condition was identified as a separate syndrome, which can be observed after severe trauma and burns, sepsis, necrotizing pancreatitis. Significant loss of muscle mass that is difficult to correct is one of the leading clinical manifestations in this case. Using literature from the MEDLINE database, modern ideas about the mechanisms of sarcopenia in the persistent inflammation, immunosuppression and catabolism syndrome and possible ways of optimal anabolic support are described.
саркопенія; запалення; катаболізм; харчова підтримка
саркопения; воспаление; катаболизм; пищевая поддержка
sarcopenia; inflammation; catabolism; nutrition
Вступ
М’язове виснаження та його механізми
Споживання білка
Анаболічні ад’юванти
Амінокислоти
Омега-3 поліненасичені жирні кислоти та SPM
Вітамін D
Висновок
- Mira J.C., Gentile L.F., Mathias B.J. et al. Sepsis pathophysiology, chronic critical illness, and persistent inflammation-immunosuppression and catabolism syndrome. Crit. Care. Med. 2017. Vol. 45. P. 253-262.
- Stortz J.A., Mira J.C., Raymond S.L. et al. Benchmarking clinical outcomes and the immunocatabolic phenotype of chronic critical illness after sepsis in surgical intensive care unit patients. J. Trauma Acute Care Surg. 2018. Vol. 84. P. 342-349.
- Gardner A.K., Ghita G.L., Wang Z. et al. The development of chronic critical illness determines physical function, quality of life, and longterm survival among early survivors of sepsis in surgical ICUs. Crit. Care Med. 2019. Vol. 47. P. 566-573
- Gentile L.F., Cuenca A.G., Efron P.A. et al. Persistent inflammation and immunosuppression: a common syndrome and new horizon for surgical intensive care. J. Trauma Acute Care Surg. 2012. Vol. 72. P. 1491-1501.
- Mira J.C., Cuschieri J., Ozrazgat-Baslanti T. et al. The epidemiology of chronic critical illness after severe traumatic injury at two level-one trauma centers. Crit. Care Med. 2017. Vol. 45. P. 1989-1996.
- Monk D.N., Plank L.D., Franch-Arcas G. et al. Sequential changes in the metabolic response in critically injured patients during the first 25 days after blunt trauma. Ann. Surg. 1996. Vol. 223. P. 395-405.
- Puthucheary Z.A., Rawal J., McPhail M., et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013. Vol. 310. P. 1591-1600.
- Wischmeyer P.E., San-Millan I. Winning the war against ICU-acquired weakness: new innovations in nutrition and exercise physiology. Crit. Care. 2015. Vol. 19, Suppl. 3. S6.
- Puthucheary Z.A., Astin R., McPhail M.J.W. et al. Metabolic phenotype of skeletal muscle in early critical illness. Thorax. 2018. Vol. 73. P. 926-935.
- Wesselink E., Koekkoek W.A.C., Grefte S. et al. Feeding mitochondria: potential role of nutritional components to improve critical illness convalescence. Clin. Nutr. 2019. Vol. 38. P. 982-995.
- Dos Santos C., Hussain S.N., Mathur S. et al. Mechanisms of chronic muscle wasting and dysfunction after an intensive care unit stay. A pilot study. Am. J. Respir. Crit. Care Med. 2016. Vol. 194. P. 821-830.
- Parry S.M., El-Ansary D., Cartwright M.S. et al. Ultrasono-graphy in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J. Crit. Care. 2015. Vol. 30. 1151. e9-1151.e14.
- Chan K.S., Mourtzakis M., Aronson Friedman L. et al. National Institutes of Health National Heart, Lung, and Blood Institute (NHLBI) Acute Respiratory Distress Syndrome (ARDS) Network. Evaluating muscle mass in survivors of acute respiratory distress syndrome: a 1-year multicenter longitudinal study. Crit. Care Med. 2018. Vol. 46. P. 1238-1246.
- Wall B.T., Dirks M.L., Snijders T. et al. Substantial skeletal muscle loss occurs during only 5 days of disuse. Acta Physiol. 2014. Vol. 210. P. 600-611.
- Gandotra S., Lovato J., Case D. et al. Physical function trajectories in survivors of acute respiratory failure. Ann. Am. Thorac. Soc. 2019. Vol. 16. P. 471-477.
- Schefold J.C., Bierbrauer J., Weber-Carstens S. Intensive care unitacquired weakness (ICUAW) and muscle wasting in critically ill patients with severe sepsis and septic shock. J. Cachexia Sarcopenia Muscle. 2010. Vol. 1. P. 147-157.
- Moro T., Ebert S.M., Adams C.M., Rasmussen B.B. Amino acid sensing in skeletal muscle. Trends Endocrinol. Metab. 2016. Vol. 27. P. 796-806.
- Bowen T.S., Schuler G., Adams V. Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J. Cachexia Sarcopenia Muscle. 2015. Vol. 6. P. 197-207.
- Gordon S.E., Lake J.A., Westerkamp C.M., Thomson D.M. Does AMP-activated protein kinase negatively mediate aged fast-twitch skeletal muscle mass? Exerc. Sport Sci. Rev. 2008. Vol. 36. P. 179-186.
- Meng S.J., Yu L.J. Oxidative stress, molecular inflammation and sarcopenia. Int. J. Mol. Sci. 2010. Vol. 11. P. 1509-1526.
- Schiaffino S., Dyar K.A., Ciciliot S. et al. Mechanisms regulating skeletal muscle growth and atrophy. FEBS J. 2013. Vol. 280. P. 4294-4314.
- Glass D.J. Skeletal muscle hypertrophy and atrophy signaling pathways. Int. J. Biochem. Cell Biol. 2005. Vol. 37. P. 1974-1984.
- Wada S., Kato Y., Okutsu M. et al. Translational suppression of atrophic regulators by microRNA-23a integrates resistance to skeletal muscle atrophy. J. Biol. Chem. 2011. Vol. 286. P. 38456-38465.
- Mourkioti F., Rosenthal N. NF-kappaB signaling in skeletal muscle: prospects for intervention in muscle diseases. J. Mol. Med. 2008. Vol. 86. P. 747-759.
- Mitch W.E., Hu Z., Lee S.W., Du J. Strategies for suppressing muscle atrophy in chronic kidney disease: mechanisms activating distinct proteolytic systems. J. Renal Nutr. 2005. Vol. 15. P. 23-27.
- Diaz M.C., Ospina-Tascon G.A., Salazar C.B. Respiratory muscle dysfunction: a multicausal entity in the critically ill patient undergoing mechanical ventilation. Arch. Bronconeumol. 2014. Vol. 50. P. 73-77.
- Tagerud S., Libelius R. Lysosomes in skeletal muscle following denervation. Time course of horseradish peroxidase uptake and increase of lysosomal enzymes. Cell Tissue Res. 1984. Vol. 236. P. 73-79.
- Singer P., Berger M.M., Van den Berghe G., Biolo G. et al. ESPEN Guidelines on Parenteral Nutrition: intensive care. Clin. Nutr. 2009. Vol. 28. P. 387-400.
- Jolliet P., Pichard C., Biolo G. et al. Enteral nutrition in intensive care patients: a practical approach. Working group on nutrition and metabolism, ESICM. European Society of Intensive Care Medicine. Intensive Care Med. 1998. Vol. 24. P. 848-859.
- Hoffer L.J., Bistrian B.R. What is the best nutritional support for critically ill patients? Hepatobil. Surg. Nutr. 2014. Vol. 3. P. 172-174.
- Moore F.A., Phillips S.M., McClain C.J. et al. Nutrition support for persistent inflammation, immunosuppression, and catabolism syndrome. Nutr. Clin. Pract. 2017. Vol. 32. Suppl. 1. S. 121-127.
- Hurt R.T., McClave S.A., Martindale R.G. et al. Summary points and consensus recommendations from the international protein summit. Nutr. Clin. Pract. 2017. Vol. 32. Suppl. 1. S. 142-151.
- Deutz N.E., Wolfe R.R. Is there a maximal anabolic response to protein intake with a meal? Clin. Nutr. 2013. Vol. 32. P. 309-313.
- Anton S.D., Hida A., Mankowski R. et al. Nutrition and exercise in sarcopenia. Curr. Protein Pept. Sci. 2018. Vol. 19. P. 649-667.
- Herndon D.N., Tompkins R.G. Support of the metabolic response to burn injury. Lancet. 2004. Vol. 363. P. 1895-1902.
- Allingstrup M.J., Esmailzadeh N., Wilkens Knudsen A. et al. Provision of protein and energy in relation to measured requirements in intensive care patients. Clin. Nutr. 2012. Vol. 31. P. 462-468.
- McClave S.A., Martindale R.G., Vanek V.W. et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). J. Parenter. Enter. Nutr. 2009. Vol. 33. P. 277-316.
- Hoffer L.J., Bistrian B.R. Appropriate protein provision in critical illness: a systematic and narrative review. Am. J. Clin. Nutr. 2012. Vol. 96. P. 591-600.
- Op den Kamp C.M., Langen R.C., Haegens A., Schols A.M. Muscle atrophy in cachexia: can dietary protein tip the balance? Curr. Opin. Clin. Nutr. Metab. Care. 2009. Vol. 12. P. 611-616.
- Bauer J., Morley J.E., Schols A.M.W.J. et al. Sarcopenia: a time for action. An SCWD Position Paper. J. Cachexia Sarcopenia Muscle. 2019. Vol. 10. P. 956-961.
- Arends J., Bachmann P., Baracos V. et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017. Vol. 36. P. 11-48.
- Deutz N.E., Matheson E.M., Matarese L.E. et al. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: a randomized clinical trial. Clin. Nutr. 2016. Vol. 35. P. 18-26.
- Stanojcic M., Finnerty C.C., Jeschke M.G. Anabolic and anticatabolic agents in critical care. Curr. Opin. Crit. Care. 2016. Vol. 22. P. 325-331.
- Porro L.J., Herndon D.N., Rodriguez N.A. et al. Five-year outcomes after oxandrolone administration in severely burned children: a randomized clinical trial of safety and efficacy. J. Am. Coll. Surg. 2012. Vol. 214. P. 489-502.
- Herndon D.N., Hart D.W., Wolf S.E. et al. Reversal of catabolism by beta-blockade after severe burns. N. Engl. J. Med. 2001. Vol. 345. P. 1223-1229.
- Suman O.E., Spies R.J., Celis M.M. et al. Effects of a 12-wk resistance exercise program on skeletal muscle strength in children with burn injuries. J. Appl. Physiol. 2001. Vol. 91. P. 1168-1175.
- Hart D.W., Herndon D.N., Klein G. et al. Attenuation of posttraumatic muscle catabolism and osteopenia by long-term growth hormone therapy. Ann. Surg. 2001. Vol. 17. P. 827-834.
- Gibran N., Wiechman S., Meyer W. et al. Summary of the 2012 ABA burn quality consensus conference. J. Burn Care Res. 2013. Vol. 34. P. 361-385.
- Jeschke M.G., Finnerty C.C., Suman O.E. et al. The effect of oxandrolone on the endocrinologic, inflammatory, and hypermetabolic responses during the acute phase postburn. Ann. Surg. 2007. Vol. 246. P. 351-360.
- Reeves P.T., Herndon D.N., Tanksley J.D. et al. Five-year outcomes after long-term oxandrolone administration in severely burned children. Shock. 2016. Vol. 45. P. 367-374.
- Giannoulis M.G., Martin F.C., Nair K.S. et al. Hormone replacement therapy and physical function in healthy older men. Time to talk hormones? Endocr. Rev. 2012. Vol. 33. P. 314-377.
- Xu L., Freeman G., Cowling B.J., Schooling C.M. Testosterone therapy and cardiovascular events among men: A systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med. 2013. Vol. 11. Article number: 108.
- Lynch G.S. Emerging drugs for sarcopenia: Age-related muscle wasting. Expert Opin. Emerg. Drugs. 2004. Vol. 9. P. 345-361.
- Stewart Coats A.J., Srinivasan V., Surendran J. et al. The ACT-ONE trial, a multicentre, randomised, double-blind, placebo-controlled, dose-finding study of the anabolic/catabolic transforming agent, MT-102 in subjects with cachexia related to stage III and IV non-small cell lung cancer and colorectal cancer: Study design. J. Cachexia Sarcopenia Muscle. 2011. Vol. 2. P. 201-207.
- Rooks D., Roubeno R. Development of Pharmacotherapies for the Treatment of Sarcopenia. J. Frailty Aging. 2019. Vol. 8. P. 120-130.
- Liebau F., Wernerman J., van Loon L.J., Rooyackers O. Effect of initiating enteral protein feeding on whole-body protein turnover in critically ill patients. Am. J. Clin. Nutr. 2015. Vol. 101. P. 549-557.
- Bear D.E., Hart N., Puthucheary Z. Continuous or intermittent feeding: pros and cons. Curr. Opin. Crit. Care. 2018. Vol. 24. P. 256-261.
- Mathias B., Delmas A.L., Ozrazgat-Baslanti T. et al. Human myeloid-derived suppressor cells are associated with chronic immune suppression after severe sepsis/septic shock. Ann. Surg. 2017. Vol. 265. P. 827-834.
- Zhu X., Pribis J.P., Rodriguez P.C., Morris S.M. Jr. et al. The central role of arginine catabolism in T-cell dysfunction and increased susceptibility to infection after physical injury. Ann. Surg. 2014. Vol. 259. P. 171-178.
- Wu G., Bazer F.W., Davis T.A. et al. Arginine metabolism and nutrition in growth, health and disease. Amino Acids. 2009. Vol. 37. P. 153-168.
- Rosenthal M.D., Vanzant E.L., Martindale R.G., Moore F.A. Evolving paradigms in the nutritional support of critically ill surgical patients. Curr. Probl. Surg. 2015. Vol. 52. P. 147-182.
- English K.L., Mettler J.A., Ellison J.B. et al. Leucine partially protects muscle mass and function during bed rest in middle-aged adults. Am. J. Clin. Nutr. 2016. Vol. 103. P. 465-473.
- Nicastro H., Artioli G.G., Costa Ados S. et al. An overview of the therapeutic effects of leucine supplementation on skeletal muscle under atrophic conditions. Amino Acids. 2011. Vol. 40. P. 287-300.
- Cynober L., De Bandt J.P., Moinard C. Leucine and citrulline: two major regulators of protein turnover. World Rev. Nutr. Diet. 2013. Vol. 105. P. 97-105.
- Hernandez-Garcia A.D., Columbus D.A., Manjarin R. et al. Leucine supplementation stimulates protein synthesis and reduces degradation signal activation in muscle of newborn pigs during acute endotoxemia. Am. J. Physiol. Endocrinol. Metab. 2016. Vol. 311. E. 791-801.
- Drummond M.J., Reidy P.T., Baird L.M. et al. Leucine differentially regulates gene-specific translation in mouse skeletal muscle. J. Nutr. 2017. Vol. 147. P. 1616-1623.
- Pereira M.G., Silva M.T., da Cunha F.M. et al. Leucine supplementation improves regeneration of skeletal muscles from old rats. Exp. Gerontol. 2015. Vol. 72. P. 269-277.
- Katsanos C.S., Kobayashi H., Sheffield-Moore M. et al. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Am. J. Physiol. 2006. Vol. 291. E. 381-387.
- Deutz N.E., Safar A., Schutzler S. et al. Muscle protein synthesis in cancer patients can be stimulated with a specially formulated medical food. Clin. Nutr. 2011. Vol. 30. P. 759-768.
- Holecek M. Beta-hydroxy-beta-methylbutyrate supplementation and skeletal muscle in healthy and muscle-wasting conditions. J. Cachexia Sarcopenia Muscle. 2017. Vol. 8. P. 529-541.
- Rosenthal M.D., Rosenthal C.M., Moore F.A., Martindale R.G. Persistent immunosuppression, inflammation, catabolism syndrome and diaphragmatic dysfunction. Curr. Pulmonol. Rep. 2017. Vol. 6. P. 54-57.
- Delphan M., Lin T., Liesenfeld D.B. et al. Associations of branched chain amino acids with parameters of energy balance and survival in colorectal cancer patients: results from the ColoCare Study. Metabolomics. 2018. 2018(14). 22.
- Nissen S.L., Abumrad N.N. Nutritional role of the leucine metabolite β-hydroxy β-methylbutyrate (HMB). J. Nutr. Biochem. 1997. Vol. 8. P. 300-311.
- Smith K.L., Tisdale M.J. Increased protein degradation and decreased protein synthesis in skeletal muscle during cancer cachexia. Br. J. Cancer. 1993. Vol. 67. P. 680-685.
- Bear D.E., Langan A., Dimidi E. et al. β-hydroxy-β-methylbutyrate and its impact on skeletal muscle mass and physical function in clinical practice: a systematic review and meta-analysis. Am. J. Clin. Nutr. 2019. Vol. 109. P. 1119-1132.
- Mitchell W.K., Phillips B.E., Hill I. et al. Human skeletal muscle is refractory to the anabolic effects of leucine during the postprandial muscle-full period in older men. Clin. Sci. 2017. Vol. 131. P. 2643-2653.
- De Bandt J.P. Leucine and mammalian target of rapamycin-dependent activation of muscle protein synthesis in aging. J. Nutr. 2016. Vol. 146. S. 2616-2624.
- Bergstrom J., Furst P., Noree L.O., Vinnars E. Intracellular free amino acid concentration in human muscle tissue. J. Appl. Physiol. 1974. Vol. 36. P. 693-697.
- Thomas D.T., Erdman K.A., Burke L.M. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: nutrition and athletic performance. J. Acad. Nutr. Diet. 2016. Vol. 116. P. 501-528.
- Gualano B., Rawson E.S., Candow D.G., Chilibeck P.D. Creatine supplementation in the aging population: effects on skeletal muscle, bone and brain. Amino Acids. 2016. Vol. 48. P. 1793-1805.
- Rondanelli M., Faliva M., Monteferrario F. et al. Novel insights on nutrient management of sarcopenia in elderly. Biomed. Res. Int. 2015. Vol. 2015. Article ID 524948.
- Pappalardo G., Almeida A., Ravasco P. Eicosapentaenoic acid in cancer improves body composition and modulates metabolism. Nutrition. 2015. Vol. 31. P. 549-555.
- Rosenthal M.D., Patel J., Staton K. et al. Can specialized pro-resolving mediators deliver benefit originally expected from fish oil? Curr. Gastroenterol. Rep. 2018. Vol. 20. Article 40.
- Dalli J., Colas R.A., Serhan C.N. Novel n-3 immunoresolvents: structures and actions. Sci. Rep. 2013. Vol. 3. Article 1940.
- Dalli J., Colas R.A., Quintana C. et al. Human sepsis eicosanoid and proresolving lipid mediator temporal profiles: correlations with survival and clinical outcomes. Crit. Care. Med. 2017. Vol. 45. P. 58-68.
- Serhan C.N., Dalli J., Karamnov S. et al. Macrophage proresolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. 2012. Vol. 26. P. 1755-1765.
- Chiang N., Serhan C.N. Structural elucidation and physiologic functions of specialized pro-resolving mediators and their receptors. Mol. Aspects Med. 2017. Vol. 58. P. 114-129.
- Rondanelli M., Klersy C., Terracol G. et al. Whey protein, amino acids, and vitamin D supplementation with physical activity increases fat-free mass and strength, functionality, and quality of life and decreases inflammation in sarcopenic elderly. Am. J. Clin. Nutr. 2016. Vol. 103. P. 830-840.
- Braun A.B., Gibbons F.K., Litonjua A.A. et al. Low serum 25-hydroxyvitamin D at critical care initiation is associated with increased mortality. Crit. Care Med. 2012. Vol. 40. P. 63-72.
- Higgins D.M., Wischmeyer P.E., Queensland K.M. et al. Relationship of vitamin D deficiency to clinical outcomes in critically ill patients. J. Parenter. Enter. Nutr. 2012. Vol. 36. P. 713-720.
- McKinney J.D., Bailey B.A., Garrett L.H. et al. Relationship between vitamin D status and ICU outcomes in veterans. J. Am. Med. Di. Assoc. 2011. Vol. 12. P. 208-211.
- Bauer J.M., Verlaan S., Bautmans I. et al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double blind, placebo-controlled trial. J. Am. Med. Dir. Assoc. 2015. Vol. 16. P. 740-747.
- Rosenthal M.D., Kamel A.Y., Rosenthal C.M. et al. Chronic critical illness: Application of what we know. Nutr. Clin. Pract. 2018. Vol. 33. P. 39-45.